Let’s talk about it
Lipedema is a chronic medical condition that forms a symmetrical buildup of adipose tissue (fat) in the legs, arms, and lower trunk. It often causes pain, swelling, heaviness, loose skin, easy bruising, and the feeling of nodules under the skin. These nodules often feel like rice, pearls, or walnuts under the skin.
Who gets Lipedema?
Lipedema affects almost exclusively individuals assigned female at birth (AFAB). Lipedema bodies come in various shapes and sizes. Lipedema can cause pain and disablement at any size.
When Does it Develop?
Typically around puberty, but it can also develop or become more pronounced during other hormonal changes, such as pregnancy or menopause. Hormonal birth control may also be a trigger for the onset of lipedema symptoms.
How Common is Lipedema?
Estimates suggest that up to 11% of females worldwide may have the condition. While the exact cause is unknown, genetics is believed to play a role, as it often runs in families.
Is Lipedema Painful?
Lipedema fat is often painful. People with lipedema report pain with massage, children or pets walking across their laps, or having their blood pressure taken.
Why can’t I lose Weight?
Lipedema fat is often resistant to nutritional intervention, exercise, elevation, diuretics, and bariatric surgery.
Can it Impair Mobility?
Lipedema can lead to mobility issues as it progresses. As with most conditions, the intensity of symptoms varies from person to person, mild in some, and severe in others.
Although first discovered in 1940, lipedema is still poorly understood, making diagnosis and care a source of deep frustration for patients.
Obesity
Fat distribution and composition are different in lipedema. Additionally, people with lipedema do not typically have diabetes, high cholesterol, or high blood pressure. In later stages of lipedema, obesity and lipedema can be present at the same time, but they remain two separate diseases that must be treated differently.
Fat phobia, fat bias, and gender bias are often barriers to accessing appropriate care for lipedema. Lipedema fat often does not respond to diet and exercise interventions or weight loss surgery.
Lipedema affects almost exclusively individuals assigned female at birth (AFAB). Lipedema bodies come in various shapes and sizes. Lipedema can cause pain and disablement at any size.
Lymphedema
Lymphedema generally causes swelling on only one side of the body and includes the hands and feet. Lymphedema can be diagnosed with imaging and genetic tests.
Your Fault
Lipedema is not a moral failing. It is a real medical condition that is worthy of care, compassion, and support. People with lipedema often report “knowing something isn’t right” when their bodies grow larger and more painful despite all efforts to eat nutritious foods and exercise.
Fat Accumulation
Excessive, symmetrical accumulation of fat in the legs and sometimes in the arms, sparing the hands and feet. Fat tissue often feels like pearls, rice, or walnuts under the skin. Cuffing at the ankles and wrists is frequently (but not always) present depending on the type of lipedema a person has.
Symmetry
Lipedema typically affects both sides of the body equally, unlike conditions like lymphedema, which usually present asymmetrically (on one side or one limb).
Painful Fat
Painful fat is the distinguishing characteristic of lipedema. The fat is tender to the touch with firm pressure. Patients often report that having their blood pressure measured is very painful or that they experience discomfort when pets or children walk on their laps. This pain and tenderness are unique to lipedema. Each individual experiences pain differently, and the range of pain and discomfort can vary from person to person.
Easy Bruising
The skin may bruise easily, even with minor trauma. Sometimes we refer to these as “bruises of unknown origin,” as patients may have many bruises primarily on the affected areas with no clear idea of what caused them.
Swelling
Affected areas may appear swollen or puffy. The swelling is usually more pronounced after long periods of standing or toward the end of the day. Typically, the swelling resolves overnight or with leg elevation. Lipedema swelling is non-pitting, meaning it does not leave an indentation in the skin when pressed with fingers.
Impacts Mobility
Lipedema can lead to decreased mobility. Walking or standing for long periods is often painful. Mobility can be impacted at any stage and size.
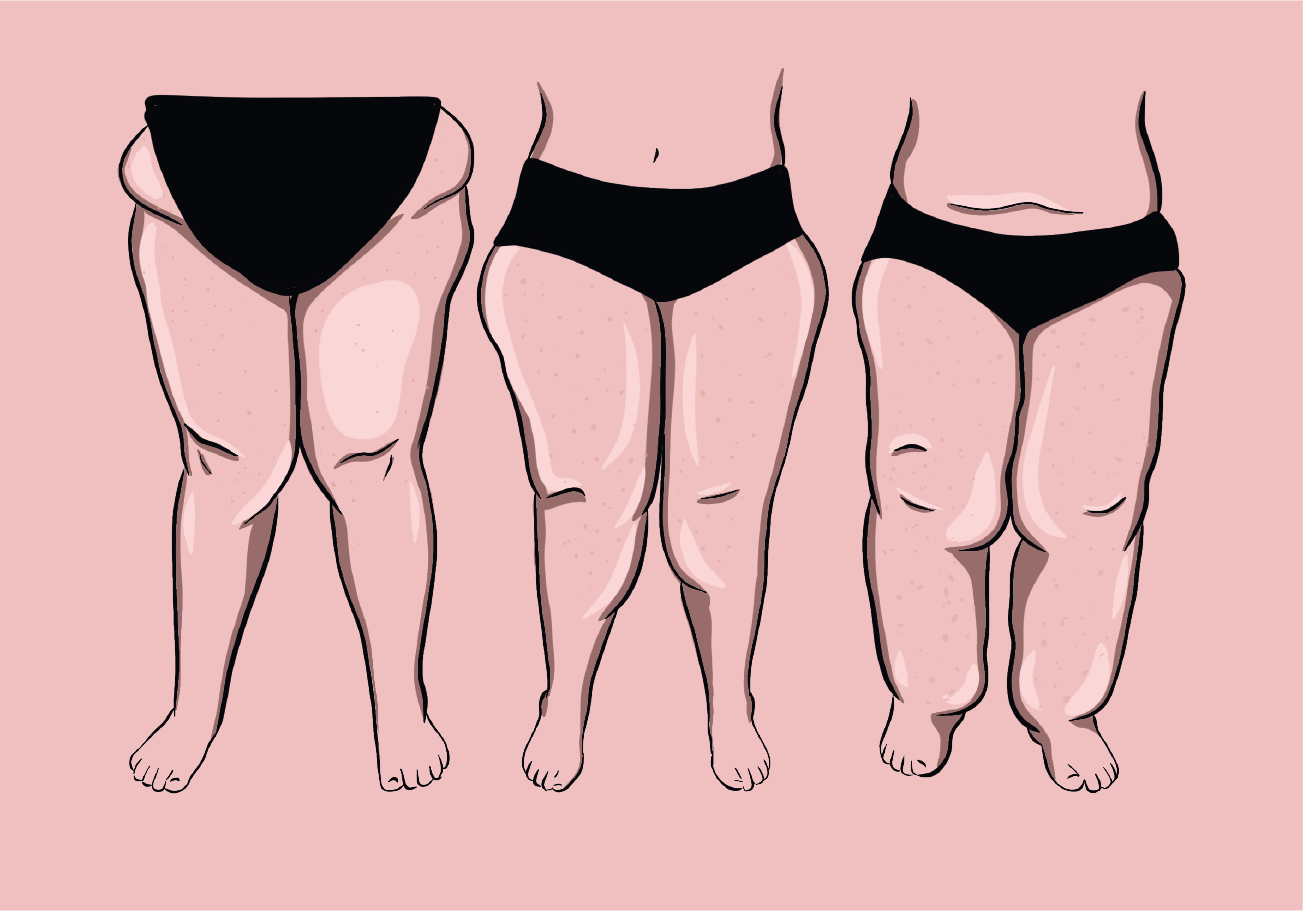
‘Stage’ refers to the advancement of symptoms and progression of the disease. Pain and dysfunction can be present at every stage and body size.
Stage 1: Skin has a smooth texture with a pebble-like feel beneath the skin due to underlying loose connective tissue fibrosis.
Stage 2: Patients have more lipedema tissue than those with Stage 1. Skin is now dimpling (appears like cellulite) due to progressed fibrotic changes and excess tissue. Palpable nodules may be larger and more numerous.
Stage 3: Significantly increased lipedema tissue, more fibrotic in texture, with numerous large nodules beneath the skin. Overhanging lobules of tissue now change the normal anatomy of the affected areas.
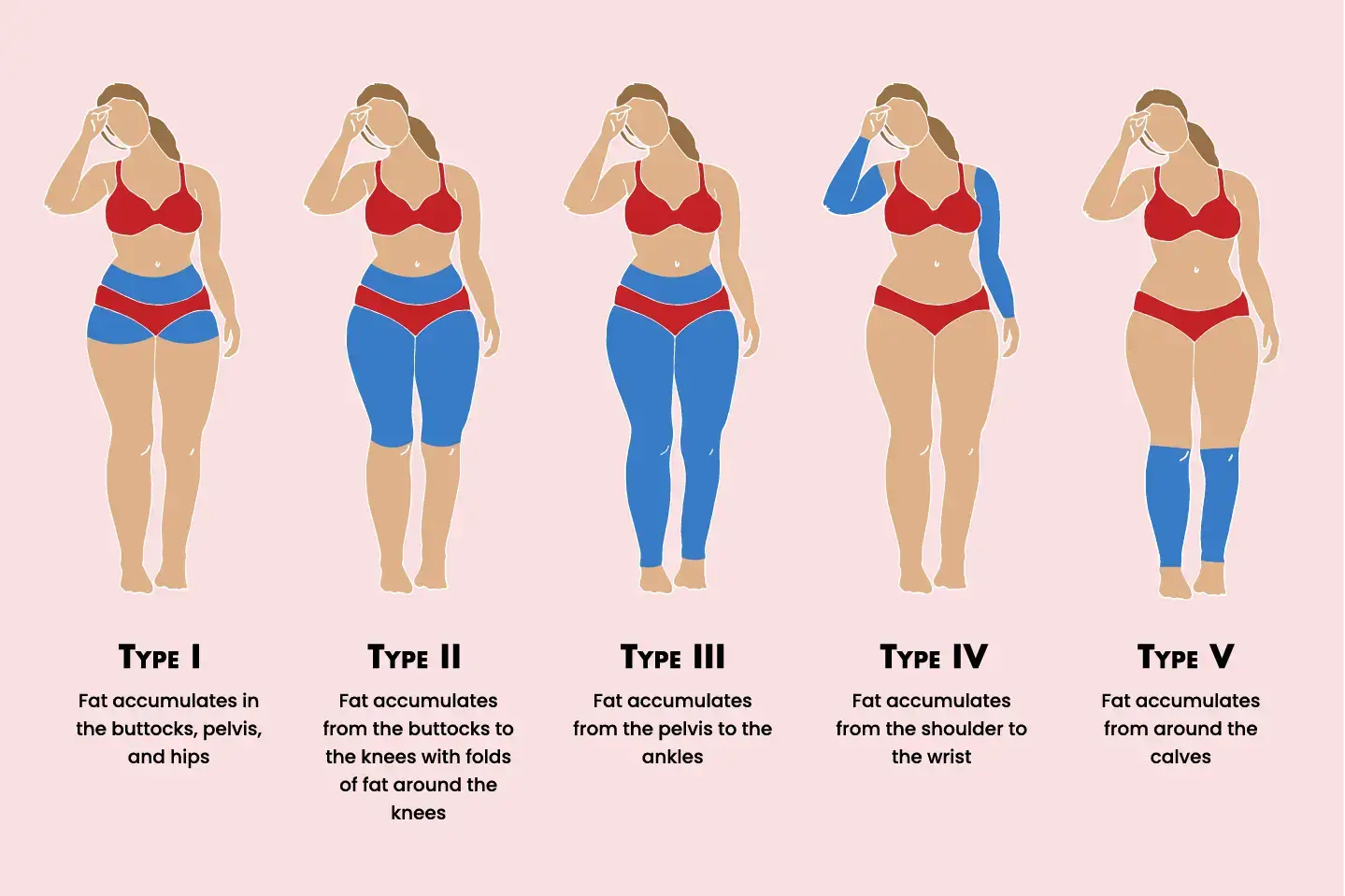
‘Types’ of lipedema refer to the areas of the body affected by lipedema fat accumulation.
Lipedema has five main types and often people with lipedema may have a combination of types. For example: Type III/IV is a person who is affected by lipedema from the pelvis to the ankles as well as the arms. Many persons with lipedema do not fit neatly into just one category.
Type I: Fat accumulation in the buttocks, pelvis, and hips
Type II: Fat accumulation from the buttocks to the knees with folds of fat around the knees (medial knee fat pads)
Type III: Fat accumulates from the pelvis to the ankles
Type IV: Fat accumulates from the shoulder to the wrist
Type V: Fat accumulates around the calves
While there is currently no cure for lipedema, various treatments can significantly improve mobility and quality of life. All management strategies focus on providing symptom relief.
Combined Decongestive Therapy (CDT) This involves Manual Lymphatic Drainage (MLD) performed by a certified therapist. Bandaging or wrapping may also be necessary if there is excess fluid or if lymphedema is present.
Compression Garments Class II flat-knit, made-to-measure medical-grade compression is generally recommended. However, as coverage varies by province and insurance plans, the best compression is simply the kind you can afford and will wear consistently.
Decreasing Inflammation Adopting an anti-inflammatory diet and identifying food triggers can help manage pain. Prioritizing stress management, adequate sleep, and hydration will also improve the body’s inflammatory response.
Weight Management Lipedema fat is often resistant to standard diet and exercise. However, weight management helps reduce strain on the lymphatic system. Setting realistic goals, potentially with the help of obesity medicine specialists, is key to limiting disease progression.
Low Impact Exercise Swimming, cycling, and walking are often well tolerated. Because hyper-mobile joints are common in those with lipedema, choose joint-safe activities and consult a professional before starting a new routine.
Self-Care Daily home management can include tools such as dry brushing, vibration plates, and pneumatic compression devices.
Mental Health Support Managing a chronic illness can take a heavy toll. Connecting with mental health professionals is a vital part of getting the support you need.
Lipedema Reduction Surgery Specialized surgery can significantly reduce pain, limb size, and bruising while improving mobility. This requires a surgeon with specific training in the lymphatic system. Due to a shortage of experienced providers in Canada, many patients seek qualified surgeons internationally.
Disclaimer: Lipedema Canada is not a medical provider. This guide is for informational purposes only and is not intended to substitute for professional medical advice, diagnosis, or treatment. Seek the advice of your physician regarding a medical condition or treatment before undertaking any new healthcare regimen.